Celebration at the National TB Center for Children's day in 2019. Photo: Marion Biremon / UNDP Kyrgyzstan
Fifteen year-old Anvar slowly rode his bicycle home when his mother called for dinner. Seeing this young, handsome, energetic and determined young man, a stranger could never tell that the boy finished his tuberculosis (TB) treatment just four months ago. Anvar fell sick with TB at the age of 14. He already erased this difficult moment of his life from his memory, but he remembers how hard and painful it was to breathe.
Regardless of his illness, Anvar was, somehow, lucky. His relatives accepted his diagnosis and didn’t give up on him. On the contrary, they accompanied him to the doctor and supported him at each step of his fight. After six months of treatment, Anvar was declared cured and now he even plays football with his friends. “You just have to find the patience to take all of the medication. I never wanted to stop treatment, and I’m glad I didn’t” he says, hurrying up to go back outside before it gets too dark.
In 2019, 314 children were registered with tuberculosis in the Kyrgyz Republic, but only 29 % of them (92) had bacteriological confirmation for their diagnosis.
Photo: personal archive
The importance of timely diagnosis
Tuberculosis is a curable disease if it is diagnosed and treated on time. Unfortunately, for many children that is not the case. Because TB in children can cause a multitude of symptoms, sometimes similar to other diseases, it is often diagnosed late and children can develop dangerous forms of the disease.
“Children don’t necessarily have a cough when they are sick with tuberculosis,” explains Aysalkyn Teshebaeva, head of the pediatric ward of the National TB Center in Bishkek. “What should worry parents and push them to get a consultation is a change in their child’s behavior. When they get infected with TB, young children can start becoming overactive or on the contrary become passive, and they can be capricious. For example, they may stop liking food that they enjoyed before. You may also notice some humidity behind their head and on their pillow in the morning. Even if they have a good appetite, they may not gain weight,” says Aysalkyn Teshebaeva. Expressive TB symptoms (night sweats, coughing for two weeks or more, fever, loss of weight and loss of appetite), a change in behavior or having been in contact with a TB patient should push parents to seek medical help and ask for TB testing.
Late diagnosis worsened due to Covid-19
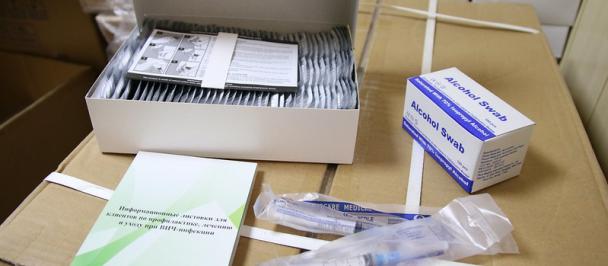
Under the Global Fund grant, the UNDP supports diagnosis and treatment of childhood TB and finances computerized tomography (CTs) for children who may have TB. This painless diagnosis method allows to confirm the suspected diagnosis in little time, before clear symptoms may appear and before the disease gets too difficult to treat. In 2019, 616 children and teenagers were tested for TB with a CT thanks to the UNDP, and 157 of them were started on treatment after the diagnosis was confirmed.
Unfortunately, diagnosis for childhood TB and TB overall has collapsed in the midst of the Covid-19 pandemic and the quarantine measures taken to limit the spread of the new virus. “Since the beginning of the new pandemic, we have had no new consultations or diagnosis for TB,” worries Aysalkyn Teshebaeva. “Now all attention is turned towards Covid-19. People don’t seek medical help unless they are in a critical state. Some of the pediatric hospitals who sent their patients to us for TB diagnosis are under quarantine,” she says, hoping that this will not too dramatically worsen the situation with childhood TB in the country.
A child taking TB treatment at the National TB Center, Bishkek. Photo: Marion Biremon / UNDP Kyrgyzstan
Screening household contacts
UNDP case managers throughout the country continue to stay in contact with TB patients and their household contacts. Their role is not only to support patients and make sure that they complete their treatment, but also to inform household contacts and regularly screen them for TB. In the region of Batken, Jyrgalbek has had to wait for more than two months to be able to bring two children to Osh to get a CT.
“The children, 6 and 10 year old, needed to get an MRI to confirm their TB diagnosis and start treatment as soon as possible. But we had to wait the end of the emergency state to bring them to Osh,” says Jyrgalbek, their case manager. All of the other family members have or had TB. “They live in very poor conditions, in one dark room that they don’t ventilate enough, and they don’t have a lot of resources. Their aunt completed her treatment but isn’t fully cured, and the others on treatment show slow results because they eat poorly,” says Jyrgalbek.
Aisalkyn Teshebaeva, medical specialist at National TB Center. Photo: Marion Biremon / UNDP Kyrgyzstan
He checks up on them often, organizes humanitarian aid distribution via several NGOs, educates them about TB and monitors their treatment. “The children don’t have any symptoms. But I asked them to do a Mantous test, and they had a clear reaction that indicates that they were probably infected too. I hope we can start them on treatment as soon as possible,” says Jyrgalbek, who understands the importance of timely diagnosis and treatment for TB.
Scientists around the world predict important setbacks in the achievements made in the fight against TB due to the Covid-19 pandemic. The UNDP / Global Fund Project and its partners are doing their best to minimize the consequences of the global pandemic on TB prevention, diagnosis and treatment.

 Locations
Locations